You come on shift in the ED and you find yourself working the first time with a patient that has had a Ventricular assist device for a few years. What do you need to know and the key points to remember?
History
created by Domingo Liotta at Baylor College of Medicine in Houston in 1962. The first LVAD was implanted in 1963. The first successful implantation of an LVAD was completed in 1966. Peter Houghton was the longest surviving recipient of a VAD for permanent use who completed a 91-mile charity walk, hiked in the Swiss Alps and the American West, flew in an ultra-light aircraft, and traveled extensively around the world.
Different approach that’s failed were the inflatable cuff around the aorta and Cardiomyoplasty.
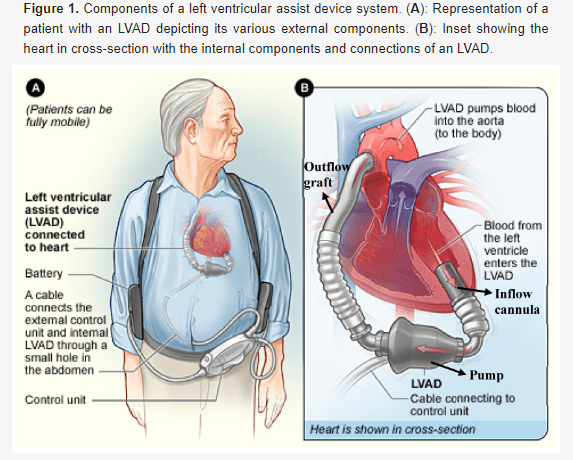
image source: https://www.mdpi.com/2077-0383/8/10/1720
Types of VAD
-Right Ventricle (RVAD) or the left ventricle (LVAD) or to both ventricles (BiVAD)
-Temporary versus permanent
-Pulsatile pumps or continuous-flow pumps
-Continuous-flow VADs are smaller and have proven to be more durable than pulsatile VADs
-Continuous flow referred to as second-generation VADs. A side effect is that the user will not have a pulse or that the pulse intensity will be seriously reduced.

Simplified Algorithm for ACLS in LVAD Patients | Creator: Shyam Murali
Key points to remember
-Many LVAD patients will not have pulses
-Get a doppler, and establish whether or not there is a MAP
-Establish perfusion not pulse
-Follow ACLS guidelines in compression and shock therapy
-LVADs are very afterload-sensitive, ^ afterload = decrease flow
Names, dates, and personal identifying details have been changed throughout this website to comply with the Health Insurance Portability and Accountability Act (HIPAA). ** | This website runs on coffee. Thank you for supporting this journey!

Leave a comment