Courtesy of Critical RN skills | https://youtu.be/RWEVGgBZ9Sg?si=Efzd-NJOKOxSgOel |
2 person prime the system. All tubing system must remain sterile when connecting and flushing.
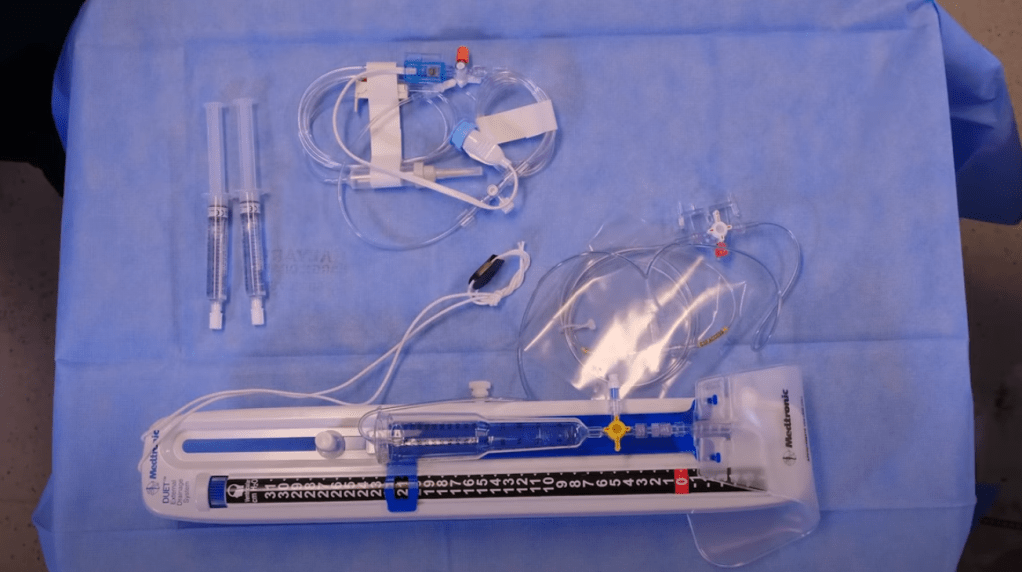
image: Sterile flush, transducer, stopcock, and the EVD with drainage system.
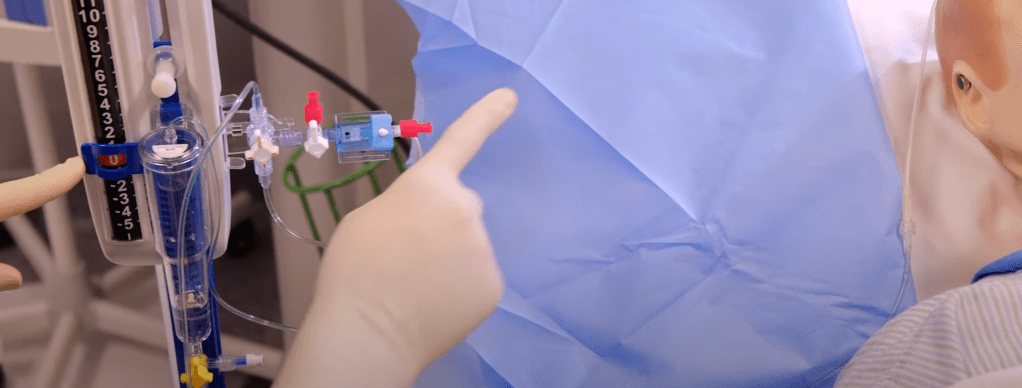
Connect primary stopcock to the system.
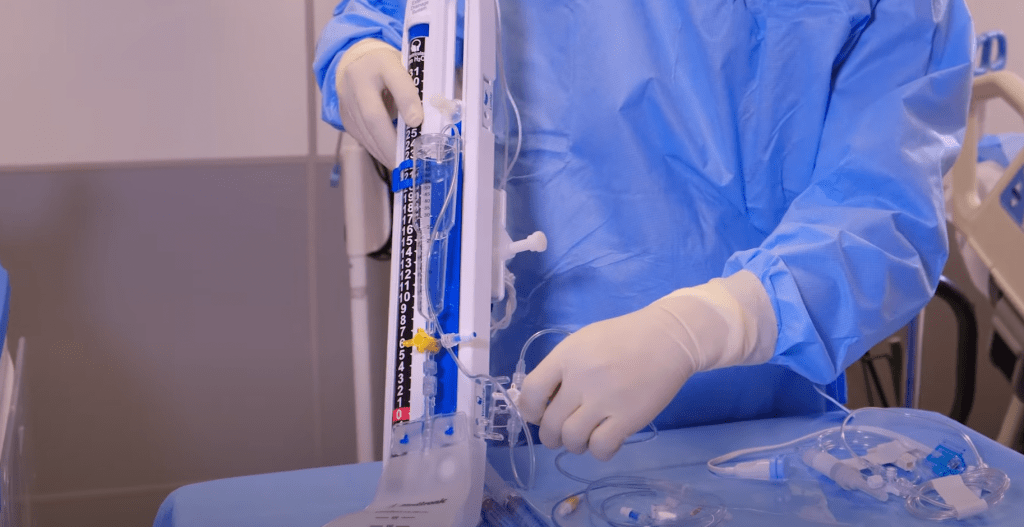
Connect transducer to main system stopcock.

MD will flush the system with sterile normal saline before connecting to patient making sure there is no air bubble to the system.
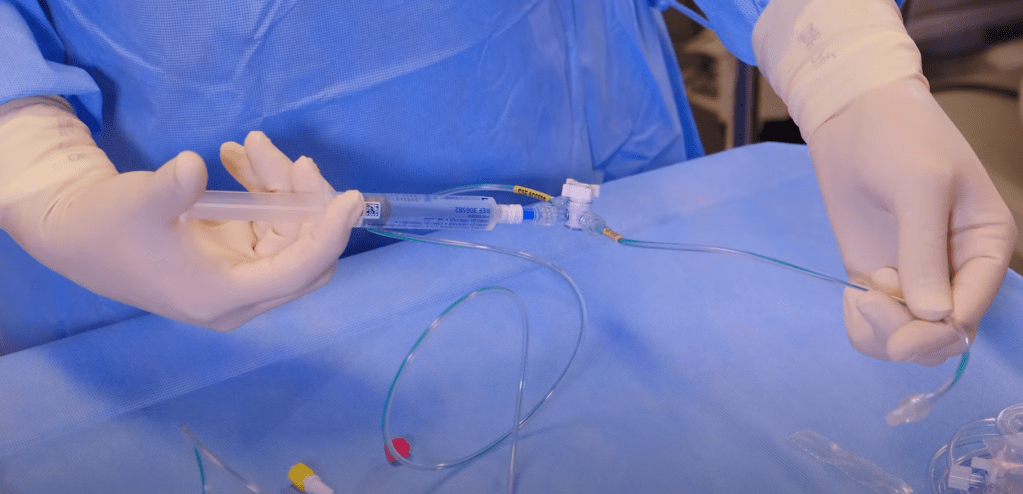
Cap the transducer with new non vented caps (red on this photo).

Connect transducer with cable.
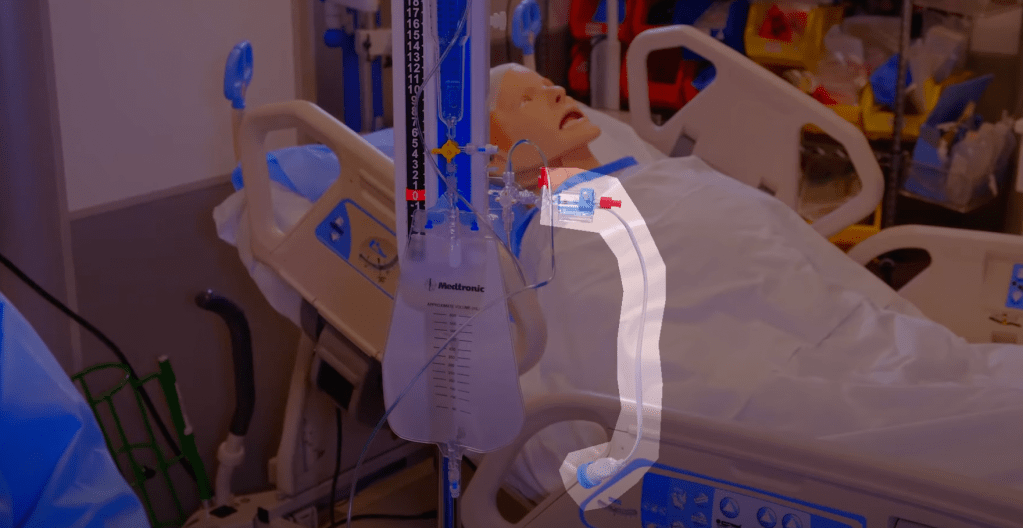
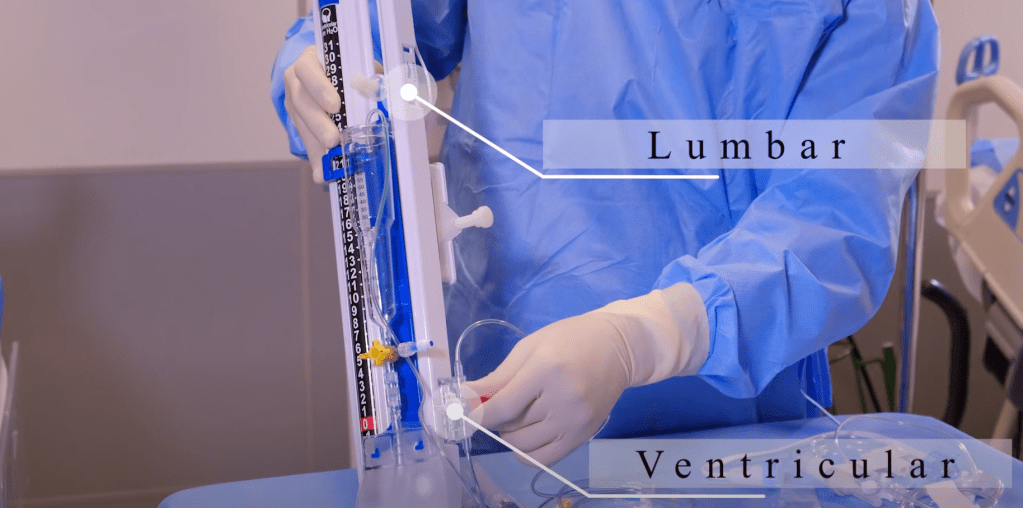
Level transducer “0” to the foramen of Monro using the tragus as a landmark.
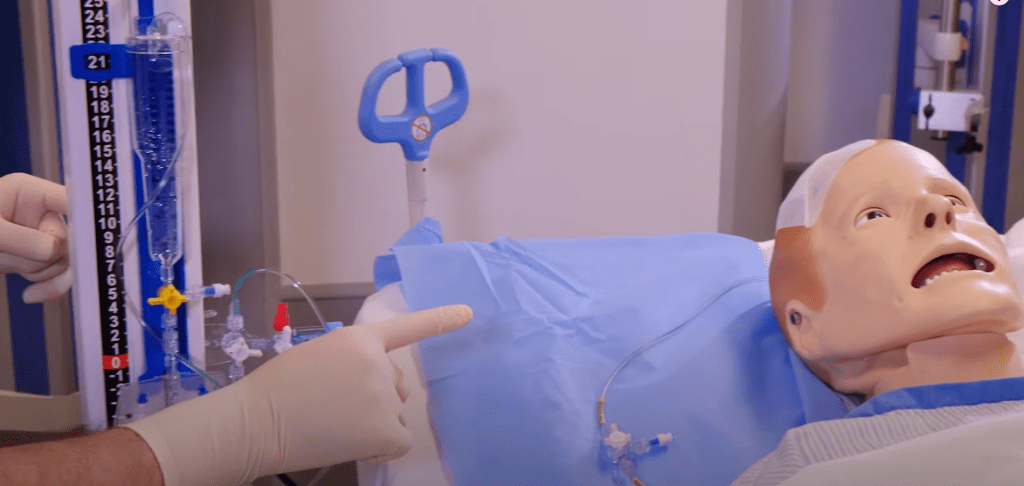

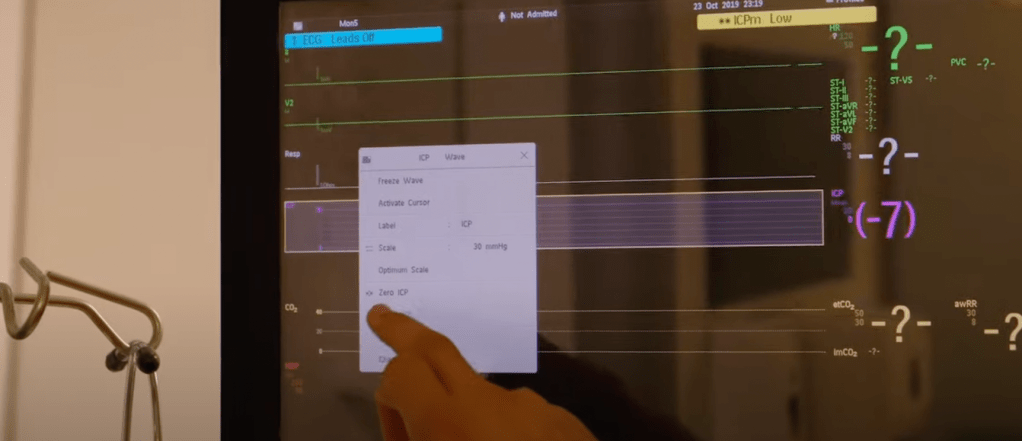
To obtain ICP reading, close off to patient then level 0 with drainage level and to patient foramen of Monro.

Zero on the monitor.
Before obtaining ICP reading, return to prescribed pressure level.
Then open between patient and the transducer side.

Key points for safe and effective care when caring for a patient with an External Ventricular Drain
1. Maintaining the EVD System Level:
- Zeroing: The EVD system must be aligned with the patient’s anatomical reference point, typically the tragus of the ear when lying flat or the mid-sagittal line between the eyebrows when on their side.
- Re-leveling: The EVD level must be adjusted whenever the patient moves to ensure accurate ICP monitoring and CSF drainage.
2. Hourly Monitoring and Documentation:
- CSF Drainage: Regularly check the CSF drainage amount to avoid complications from over- or under-drainage. An average hourly drainage rate of 10-15 ml is considered normal. However, the specific rate can vary based on individual patient needs and the physician’s orders.
- CSF Characteristics: Check the color and clarity of the CSF; any changes may show bleeding or infection.
- System Patency: Ensure the EVD system is patent, checking for CSF oscillation in the tubing and ensuring the catheter is not kinked or blocked.
- Insertion Site: Inspect the EVD insertion site for any signs of leakage, which could increase the risk of infection.
3. Neurological Assessment:
- Frequent Monitoring: Perform frequent neurological checks (at least hourly) to detect any changes in the patient’s level of consciousness, motor function, or other signs of increased intracranial pressure (ICP).
- Early Signs of Complications: Be vigilant for signs of increased ICP (headache, nausea/vomiting, decreased level of consciousness) or over-drainage (headaches).
4. Infection Prevention:
- Aseptic Technique: Strict aseptic technique must be used when handling any part of the EVD system, including the stopcock or drainage bag.
- Site Care: Ensure the dressing is intact, clean, and dry, and change it using sterile technique if needed.
- Minimize Manipulation: Avoid unnecessary manipulation of the EVD system and tubing.
- CSF Sampling: Follow institutional protocols for CSF sampling, and only do so when necessary using sterile technique.
5. System Management:
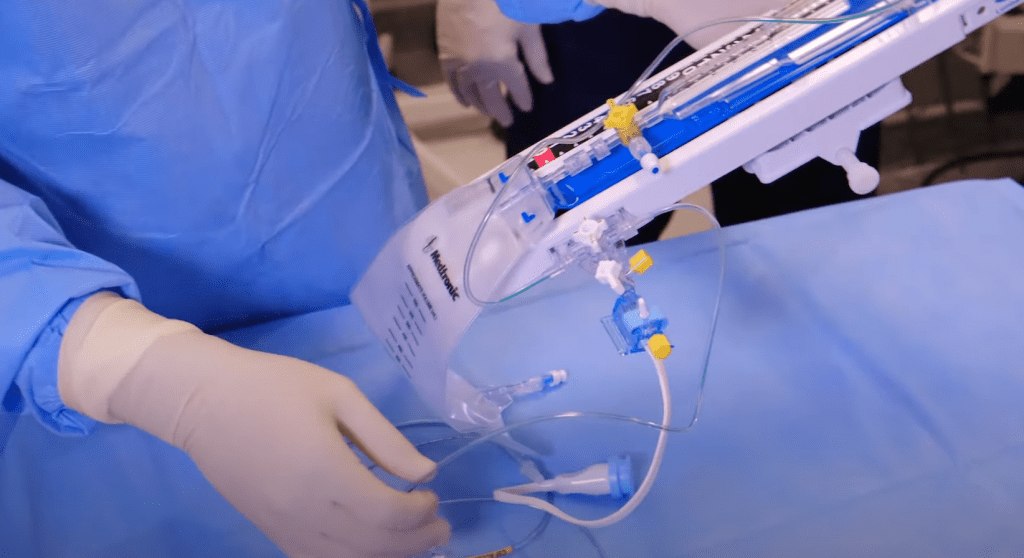
- Secure Attachment: Ensure the EVD collection system is securely attached to a dedicated pole to prevent accidental dislodgment.
- Clamping: Clamp the EVD system during patient movement or transport to prevent accidental over-drainage.
- Report Complications: Promptly report any significant changes in CSF drainage, patient condition, or signs of complications (infection, blockage, hemorrhage) to the neurosurgical team.
6. Patient and Family Education:
- Education: Provide patients and their families with education about the EVD, including the importance of maintaining the correct position, the risks of complications, and when to notify the nursing staff.
- Safety Reminders: Use signage in the room to remind staff and visitors about important EVD precautions.
7. Specific Considerations:
- CSF Leakage: Immediately report any visible CSF leakage from the insertion site to the neurosurgical team, as this poses an infection risk.
- Medication Administration: If medications are administered into the EVD, clamp the drain for the prescribed time to allow for adequate circulation.
By following these key points, nurses can ensure optimal care and management of patients with EVDs, minimizing the risk of complications and promoting positive patient outcomes.
Names, dates, and personal identifying details have been changed throughout this website to comply with the Health Insurance Portability and Accountability Act (HIPAA). **

Leave a comment